Relations list
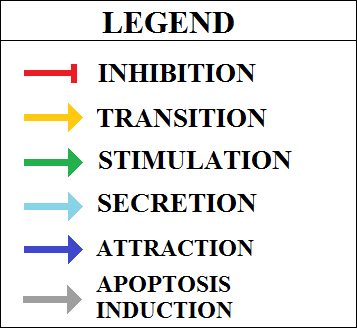
| Source |
Effect |
Target |
Tissue |
PMID |
|---|
| Activated FAP | transition | Activated FAP->Adipocyte |
Skeletal muscle |
23582327 |
| FAPs, which do not arise from the myogenic lineage, are bipotential cells capable of giving rise to fibroblasts and adipocytes |
|---|
| Activated FAP | transition | Activated FAP->Fibroblast |
Skeletal muscle |
23582327 |
| FAPs, which do not arise from the myogenic lineage, are bipotential cells capable of giving rise to fibroblasts and adipocytes |
|---|
| Activated FAP | transition | Activated FAP->Myoblast |
Skeletal muscle |
24682306 |
| Collectively, these data support the conclusion that, in addition to the reported ability to support the myogenic potential of MuSCs, FAPs from young mdx mice show a “latent” myogenic phenotype that is derepressed by HDACis at the expense of their fibro-adipogenic potential. |
|---|
| Activated FAP | transition | Activated FAP->Osteocyte |
Skeletal muscle |
28842904 |
| This multipotent progenitor population is distinct from satellite cells and is capable of fibroblastic, adipogenic, chondrogenic, and osteogenic differentiation |
|---|
| Activated FAP | secretes | COL1A1 |
Skeletal muscle |
24232182 |
| FAPs are major contributors to the deposition of several extracellular proteinsfor instance, certain collagen isoforms that are abundant in the supportive transitional ECM during muscle regeneration [65]. |
|---|
| Activated FAP | secretes | COL3A1 |
Skeletal muscle |
24232182 |
| FAPs are major contributors to the deposition of several extracellular proteinsfor instance, certain collagen isoforms that are abundant in the supportive transitional ECM during muscle regeneration [65]. |
|---|
| Activated FAP | secretes | FST |
Skeletal muscle |
23505062 |
| ability to promote differentiation of adjacent satellite cells, through upregulation of the soluble factor follistatin. |
|---|
| Activated FAP | secretes | IL33 |
Skeletal muscle |
28163303 |
| This influence is further enhanced by the recruitment of Treg cells to regenerated muscle by IL-33 released by fibro-adipogenic progenitor -FAP- cells and possibly by macrophages. |
|---|
| Activated FAP | secretes | IL6 |
Skeletal muscle |
20081841 |
| This cell type also secretes high levels of IL-6, which promotes the differentiation of myogenic cells |
|---|
| Activated FAP | secretes | WISP |
Skeletal muscle |
30686765 |
| Using transcriptomic profiling, we identify WNT1 Inducible Signaling Pathway Protein 1 (WISP1) as a FAP-derived matricellular signal that is lost during aging. WISP1 is required for efficient muscle regeneration and controls the expansion and asymmetric commitment of MuSCs through Akt signaling |
|---|
| Activated FAP->Adipocyte | transition | Adipocyte |
Skeletal muscle |
22307978 |
| Intramuscular transplantation, together with clonal analysis in culture, revealed that these progenitors are multipotent, exhibiting the capacity for both BMP-dependent skeletogenic differentiation and spontaneous adipogenic differentiation |
|---|
| Activated FAP->Fibroblast | transition | Fibroblast |
Skeletal muscle |
22307978 |
| colonies derived from single, FACS-sorted, progenitors exhibited both BMP2-dependent osteogenic differentiation and BMP2-independent adipogenic and smooth muscle/fibroblastic differentiation |
|---|
| Activated FAP->Myoblast | transition | Myoblast |
Skeletal muscle |
24682306 |
| Collectively, these data support the conclusion that, in addition to the reported ability to support the myogenic potential of MuSCs, FAPs from young mdx mice show a “latent” myogenic phenotype that is derepressed by HDACis at the expense of their fibro-adipogenic potential. |
|---|
| Activated FAP->Osteocyte | transition | Osteocyte |
Skeletal muscle |
24232182 |
| FAPs are mesenchymal stem cells resident in skeletal muscle that have the ability to differentiate into fibroblasts, adipocytes and possibly into bone and cartilage cells, although not into satellite cells or muscle fibres. |
|---|
| Activated satellite | transition | Activated satellite->Myoblast |
Skeletal muscle |
22493066 |
| In mature resting muscles, satellite cells are predominantly quiescent. Upon muscle injury, satellite cells are activated, enter the cell cycle, and proliferate. The proliferating satellite cells, called myoblasts, subsequently withdraw from the cell cycle to either differentiate or self-renew |
|---|
| Activated satellite | secretes | FN1 |
Skeletal muscle |
23290138 |
| Taken together, these results demonstrate that cell-autonomous expression of FN by activated satellite cells within their niche is indispensable for the homeostatic regulation of the satellite cell pool size during regenerative myogenesis |
|---|
| Activated satellite->Myoblast | transition | Myoblast |
Skeletal muscle |
22493066 |
| In mature resting muscles, satellite cells are predominantly quiescent. Upon muscle injury, satellite cells are activated, enter the cell cycle, and proliferate. The proliferating satellite cells, called myoblasts, subsequently withdraw from the cell cycle to either differentiate or self-renew |
|---|
| ANGPT1 | stimulates | Quiescent satellite |
Skeletal muscle |
30016618 |
| However, experiments suggested that pericytes specifically express Ang-1 and IGF-1 to regulate MuSC activation and myofiber hypertrophy, respectively |
|---|
| AREG | stimulates | Activated satellite->Myoblast |
Skeletal muscle |
28163303 |
| AREG release by Treg cells increases the expression of myogenicregulatory factors that drive the later stages of muscle differentiation. |
|---|
| AREG | stimulates | M1 macrophage->M2 macrophage |
Skeletal muscle |
28163303 |
| M1 macrophage populations then undergo a shift to a population that is biased towards the M2 pro-regenerative phenotype. Several ligands have important roles in promoting this phenotypic shift, including fibrinogen, amphiregulin -AREG- and interleukin-10 produced by regulatory T cells. |
|---|
| ARG1 | stimulates | Fibroblast |
Skeletal muscle |
28163303 |
| ARG1 has an important role in fibrosis via its metabolism of arginine to yield polyamines, which stimulate fibroblast proliferation |
|---|
| CCL2 | stimulates | Monocyte |
Skeletal muscle |
24232182 |
| Neutrophils promote the proinflammatory environment that is necessary for the clearance of cellular debris. Under certain conditions, this cell type has been suspected to transiently aggravate tissue damage. Neutrophils also secrete the chemokines MIP-1a, MCP-1 and others that favour the recruitment of monocytes |
|---|
| CCL2 | stimulates | Neutrophil |
Skeletal muscle |
28163303 |
| Resident macrophages (that express F4/80, LY6C and CD11b, but lack expression of CXC-chemokine receptor 1 (CXCR1)) promote this marked neutrophil influx by releasing the neutrophil chemoattractants CXC-chemokine ligand 1 (CXCL1) and CC-chemokine ligand 2 -CCL2- |
|---|
| CCL3 | stimulates | Monocyte |
Skeletal muscle |
24232182 |
| Neutrophils promote the proinflammatory environment that is necessary for the clearance of cellular debris. Under certain conditions, this cell type has been suspected to transiently aggravate tissue damage. Neutrophils also secrete the chemokines MIP-1a, MCP-1 and others that favour the recruitment of monocytes |
|---|
| COL1A1 | stimulates | ECM |
Skeletal muscle |
22045730 |
| Furthermore, both in vitro and in vivo experiments show that PDGFRa+ cells exclusively express fibrosis markers, such as collagen types I and III, and connective tissue growth factor |
|---|
| COL1A2 | stimulates | ECM |
Skeletal muscle |
22045730 |
| Furthermore, both in vitro and in vivo experiments show that PDGFRa+ cells exclusively express fibrosis markers, such as collagen types I and III, and connective tissue growth factor |
|---|
| COL6A1 | stimulates | ECM |
Skeletal muscle |
24232182 |
| Moreover, macrophages also secrete different ECM proteins according to the stage of macrophage differentiation. For example, M2 macrophages secrete a more mature form of fibronectin and a higher amount of ColVI than do M1 macrophages. The ECM proteins secreted by M2 macrophages are important components of the muscle stem cell niche and promote self-renewal of satellite cells |
|---|
| CXCL1 | stimulates | Neutrophil |
Skeletal muscle |
20219869 |
| Several observations support the possibility that CXCL1 or CXCL5 release from activated or mechanically perturbed muscles may contribute to activating the Th1 response to injured muscle and subsequent muscle regeneration. First, induction and release of the chemokines is rapid; both were present at elevated concentrations in the media of stimulated muscles within 3 h of stimulation (76). In addition, both chemokines are chemoattractant to neutrophils, which become significantly elevated in muscle within a few hours of injury, and they would be sufficient to drive further the Th1 inflammatory response |
|---|
| CXCL1 | stimulates | Neutrophil |
Skeletal muscle |
28163303 |
| Resident macrophages (that express F4/80, LY6C and CD11b, but lack expression of CXC-chemokine receptor 1 (CXCR1)) promote this marked neutrophil influx by releasing the neutrophil chemoattractants CXC-chemokine ligand 1 (CXCL1) and CC-chemokine ligand 2 -CCL2- |
|---|
| CXCL5 | stimulates | Neutrophil |
Skeletal muscle |
20219869 |
| Several observations support the possibility that CXCL1 or CXCL5 release from activated or mechanically perturbed muscles may contribute to activating the Th1 response to injured muscle and subsequent muscle regeneration. First, induction and release of the chemokines is rapid; both were present at elevated concentrations in the media of stimulated muscles within 3 h of stimulation (76). In addition, both chemokines are chemoattractant to neutrophils, which become significantly elevated in muscle within a few hours of injury, and they would be sufficient to drive further the Th1 inflammatory response |
|---|
| Damaged myofiber | secretes | CXCL1 |
Skeletal muscle |
20219869 |
| Several observations support the possibility that CXCL1 or CXCL5 release from activated or mechanically perturbed muscles may contribute to activating the Th1 response to injured muscle and subsequent muscle regeneration. First, induction and release of the chemokines is rapid; both were present at elevated concentrations in the media of stimulated muscles within 3 h of stimulation (76). In addition, both chemokines are chemoattractant to neutrophils, which become significantly elevated in muscle within a few hours of injury, and they would be sufficient to drive further the Th1 inflammatory response |
|---|
| Damaged myofiber | secretes | CXCL5 |
Skeletal muscle |
20219869 |
| Several observations support the possibility that CXCL1 or CXCL5 release from activated or mechanically perturbed muscles may contribute to activating the Th1 response to injured muscle and subsequent muscle regeneration. First, induction and release of the chemokines is rapid; both were present at elevated concentrations in the media of stimulated muscles within 3 h of stimulation (76). In addition, both chemokines are chemoattractant to neutrophils, which become significantly elevated in muscle within a few hours of injury, and they would be sufficient to drive further the Th1 inflammatory response |
|---|
| Damaged myofiber | attracts | Eosinophil |
Skeletal muscle |
24232182 |
| Muscle damage results in rapid recruitment of eosinophils, which secrete IL-4 to activate the regenerative actions of muscle resident fibro/adipocyte progenitors (FAPs) |
|---|
| Damaged myofiber | attracts | Mast cell |
Skeletal muscle |
24232182 |
| In resting conditions, adult skeletal muscle contains different types of resident leukocyte. The most abundant are mast cells and macrophages. These resident cell types, in conjunction with patrolling circulatory monocytes, act as sensors for distress and secrete a number of chemoattractive molecules following muscle injury. Particularly, damage-activated mast cells almost instantly begin to secrete TNF-a, histamine and tryptase and then initiate the de novo synthesis of other cytokines, such as interleukin-6 |
|---|
| Damaged myofiber | attracts | Monocyte |
Skeletal muscle |
24232182 |
| In resting conditions, adult skeletal muscle contains different types of resident leukocyte. The most abundant are mast cells and macro phages. These resident cell types, in conjunction with patrolling circulatory monocytes, act as sensors for distress and secrete a number of chemo attractive molecules following muscle injury. Beyond the first day after injury, monocytes gradually become the predominant leukocytes in the exudate. |
|---|
| Damaged myofiber | attracts | Treg |
Skeletal muscle |
27479876 |
| New studies show that injured muscle is also infiltrated by a specialized population of regulatory T cells, which control both the inflammatory response, by promoting the M1-to-M2 switch, and the activation of satellite cell |
|---|
| ECM | stimulates | FGF2 |
Skeletal muscle |
25047058 |
| Heparan sulfate proteoglycans (HSPGs) interact with a large number of growth factors in the muscle BL including insulin-like growth factor (IGF), fibrobast growth factor (FGF), hepatocyte growth factor (HGF) and transforming growth factor beta (TGF-?), all known to influence SC proliferation and differentiation (53, 54). HSPGs can increase the local concentration of growth factors, or sequester them away from cells and even participate in their function by complexing with them, dramatically affecting the local environment and driving cell behavior. |
|---|
| ECM | stimulates | HGF |
Skeletal muscle |
25047058 |
| Heparan sulfate proteoglycans (HSPGs) interact with a large number of growth factors in the muscle BL including insulin-like growth factor (IGF), fibrobast growth factor (FGF), hepatocyte growth factor (HGF) and transforming growth factor beta (TGF-?), all known to influence SC proliferation and differentiation (53, 54). HSPGs can increase the local concentration of growth factors, or sequester them away from cells and even participate in their function by complexing with them, dramatically affecting the local environment and driving cell behavior. |
|---|
| ECM | stimulates | IGF1 |
Skeletal muscle |
25047058 |
| Heparan sulfate proteoglycans (HSPGs) interact with a large number of growth factors in the muscle BL including insulin-like growth factor (IGF), fibrobast growth factor (FGF), hepatocyte growth factor (HGF) and transforming growth factor beta (TGF-?), all known to influence SC proliferation and differentiation (53, 54). HSPGs can increase the local concentration of growth factors, or sequester them away from cells and even participate in their function by complexing with them, dramatically affecting the local environment and driving cell behavior. |
|---|
| ECM | stimulates | Quiescent satellite |
Skeletal muscle |
12181355 |
| HGF is a heparin-binding growth factor that has been localized in the extracellular domain of uninjured skeletal muscle fibers, and after injury HGF quickly associates with satellite cells. Furthermore, quiescent and activated satellite cells have been shown to express the c-met receptor, which mediates the intracellular signaling response of HGF, which is consistent with the proposed role of HGF in activating quiescent satellite cells |
|---|
| ECM | stimulates | TGFB1 |
Skeletal muscle |
25047058 |
| Heparan sulfate proteoglycans (HSPGs) interact with a large number of growth factors in the muscle BL including insulin-like growth factor (IGF), fibrobast growth factor (FGF), hepatocyte growth factor (HGF) and transforming growth factor beta (TGF-?), all known to influence SC proliferation and differentiation (53, 54). HSPGs can increase the local concentration of growth factors, or sequester them away from cells and even participate in their function by complexing with them, dramatically affecting the local environment and driving cell behavior. |
|---|
| Eosinophil | secretes | IL13 |
Skeletal muscle |
24232182 |
| Regulation of cellular crosstalk also involves eosinophils that are recruited during the early stages of regeneration [37]. Eosinophils release the cytokines IL-4 and IL-13, which induce the proliferation of FAPs and simultaneously block their adipogenic differentiation. |
|---|
| Eosinophil | secretes | IL4 |
Skeletal muscle |
24232182 |
| Regulation of cellular crosstalk also involves eosinophils that are recruited during the early stages of regeneration [37]. Eosinophils release the cytokines IL-4 and IL-13, which induce the proliferation of FAPs and simultaneously block their adipogenic differentiation. |
|---|
| Fibroblast | secretes | COL1A1 |
Skeletal muscle |
22045730 |
| During normal wound healing in adult animals, fibroblasts initially migrate into the wound area and, as they do so, lay down a collagen- and cellular fibronectin-rich ECM |
|---|
| Fibroblast | secretes | COL1A2 |
Skeletal muscle |
22045730 |
| During normal wound healing in adult animals, fibroblasts initially migrate into the wound area and, as they do so, lay down a collagen- and cellular fibronectin-rich ECM |
|---|
| Fibroblast | secretes | FN1 |
Skeletal muscle |
24232182 |
| Fibroblasts are heterogeneous,with expression profiles that differ depending on the tissue source. A major function of this cell type is the deposition of fibrillar ECM, such as collagen and fibronectin, and basement membrane constituents |
|---|
| Fibroblast | secretes | MSTN |
Skeletal muscle |
18453534 |
| Myostatin expression in fibroblasts is not limited to muscle [...]. Myostatin produced from fibroblasts is biologically active. |
|---|
| FN1 | stimulates | Activated satellite |
Skeletal muscle |
23290138 |
| Taken together, these results demonstrate that cell-autonomous expression of FN by activated satellite cells within their niche is indispensable for the homeostatic regulation of the satellite cell pool size during regenerative myogenesis |
|---|
| FN1 | stimulates | ECM |
Skeletal muscle |
24232182 |
| Moreover, macrophages also secrete different ECM proteins according to the stage of macrophage differentiation. For example, M2 macrophages secrete a more mature form of fibronectin and a higher amount of ColVI than do M1 macrophages. The ECM proteins secreted by M2 macrophages are important components of the muscle stem cell niche and promote self-renewal of satellite cells |
|---|
| HGF | stimulates | Quiescent satellite |
Skeletal muscle |
12181355 |
| HGF is a heparin-binding growth factor that has been localized in the extracellular domain of uninjured skeletal muscle fibers, and after injury HGF quickly associates with satellite cells. Furthermore, quiescent and activated satellite cells have been shown to express the c-met receptor, which mediates the intracellular signaling response of HGF, which is consistent with the proposed role of HGF in activating quiescent satellite cells |
|---|
| IFNG | stimulates | M1 macrophage |
Skeletal muscle |
28163303 |
| Although phagocytic macrophages biased towards the M1 phenotype remove debris resulting from muscle injury, they also express IFN gamma, which may reinforce the macrophage phenotype and retain MPCs in a proliferative, non-differentiated state so that their populations can expand and support tissue repair |
|---|
| IFNG | stimulates | Quiescent satellite |
Skeletal muscle |
28163303 |
| Although phagocytic macrophages biased towards the M1 phenotype remove debris resulting from muscle injury, they also express IFN gamma, which may reinforce the macrophage phenotype and retain MPCs in a proliferative, non-differentiated state so that their populations can expand and support tissue repair |
|---|
| IGF1 | stimulates | Quiescent satellite |
Skeletal muscle |
30016618 |
| However, experiments suggested that pericytes specifically express Ang-1 and IGF-1 to regulate MuSC activation and myofiber hypertrophy, respectively |
|---|
| IL10 | stimulates | M1 macrophage->M2 macrophage |
Skeletal muscle |
28163303 |
| M1 macrophage populations then undergo a shift to a population that is biased towards the M2 pro-regenerative phenotype. Several ligands have important roles in promoting this phenotypic shift, including fibrinogen, amphiregulin -AREG- and interleukin-10 produced by regulatory T cells. |
|---|
| IL13 | stimulates | Quiescent FAP->Activated FAP |
Skeletal muscle |
24232182 |
| Eosinophils release the cytokines IL-4 and IL-13, which induce the proliferation of FAPs and simultaneously block their adipogenic differentiation |
|---|
| IL1B | stimulates | Quiescent satellite->Activated satellite |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells |
|---|
| IL33 | stimulates | Treg |
Skeletal muscle |
28163303 |
| This influence is further enhanced by the recruitment of Treg cells to regenerated muscle by IL-33 released by fibro-adipogenic progenitor -FAP- cells and possibly by macrophages. |
|---|
| IL4 | inhibits | Activated FAP->Adipocyte |
Skeletal muscle |
23582327 |
| Activation of IL-4/IL-13 signaling promotes proliferation of FAPs to support myogenesis while inhibiting their differentiation into adipocytes |
|---|
| IL4 | stimulates | Activated satellite->Myoblast |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells, whereas IL-4 and IGF-1 released by M2 macrophages promote their differentiation [43,52,53]. |
|---|
| IL4 | stimulates | Quiescent FAP->Activated FAP |
Skeletal muscle |
24232182 |
| Eosinophils release the cytokines IL-4 and IL-13, which induce the proliferation of FAPs and simultaneously block their adipogenic differentiation |
|---|
| IL5 | stimulates | Eosinophil |
Skeletal muscle |
17259966 |
| The array of mediators released by human mast cells is enormous and explains how mast cells can be involved in so many different physiological and pathophysiological functions. Of particular relevance...cytokines, such as IL-3 -basophil recruitment and activation-, IL-5 -eosinophil recruitment and activation- and IL-13 -induction of IgE synthesis by B cells- |
|---|
| IL6 | stimulates | Quiescent satellite->Activated satellite |
Skeletal muscle |
24232182 |
| At low physiological concentrations, TNF-a, tryptase and IL-6 promote activation and proliferation of satellite cells [31-33]. |
|---|
| IL6 | stimulates | Quiescent satellite->Activated satellite |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells |
|---|
| M0 macrophage->M1 macrophage | transition | M1 macrophage |
Skeletal muscle |
22378047 |
| In response to various signals, macrophages may undergo classical M1 activation (stimulated by TLR ligands and IFN-) or alternative M2 activation (stimulated by IL-4/IL-13) |
|---|
| M0 macrophage->M2 macrophage | transition | M2 macrophage |
Skeletal muscle |
22378047 |
| In response to various signals, macrophages may undergo classical M1 activation (stimulated by TLR ligands and IFN-) or alternative M2 activation (stimulated by IL-4/IL-13) |
|---|
| M1 macrophage | secretes | CCL2 |
Skeletal muscle |
28163303 |
| Resident macrophages (that express F4/80, LY6C and CD11b, but lack expression of CXC-chemokine receptor 1 (CXCR1)) promote this marked neutrophil influx by releasing the neutrophil chemoattractants CXC-chemokine ligand 1 (CXCL1) and CC-chemokine ligand 2 -CCL2- |
|---|
| M1 macrophage | secretes | CXCL1 |
Skeletal muscle |
28163303 |
| Resident macrophages (that express F4/80, LY6C and CD11b, but lack expression of CXC-chemokine receptor 1 (CXCR1)) promote this marked neutrophil influx by releasing the neutrophil chemoattractants CXC-chemokine ligand 1 (CXCL1) and CC-chemokine ligand 2 -CCL2- |
|---|
| M1 macrophage | secretes | IFNG |
Skeletal muscle |
28163303 |
| Although phagocytic macrophages biased towards the M1 phenotype remove debris resulting from muscle injury, they also express IFN gamma, which may reinforce the macrophage phenotype and retain MPCs in a proliferative, non-differentiated state so that their populations can expand and support tissue repair |
|---|
| M1 macrophage | secretes | IL1B |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells |
|---|
| M1 macrophage | secretes | IL6 |
Skeletal muscle |
23169615 |
| the proinflammatory cytokines IL-6 and IL-1 are mainly secreted by M1 MPs |
|---|
| M1 macrophage | secretes | IL6 |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells |
|---|
| M1 macrophage | transition | M1 macrophage->M2 macrophage |
Skeletal muscle |
17485518 |
| injured skeletal muscle recruits MOs exhibiting inflammatory profiles that operate phagocytosis and rapidly convert to antiinflammatory MPs that stimulate myogenesis and fiber growth |
|---|
| M1 macrophage | secretes | nitric oxide |
Skeletal muscle |
20219869 |
| Furthermore, The expression of iNOS by M1 macrophages enables them to induce further muscle damage through production of cytotoxic levels of NO |
|---|
| M1 macrophage | secretes | nitric oxide |
Skeletal muscle |
18996917 |
| For example, macrophages that are driven in vitro to a pro-inflammatory, M1 phenotype lyse muscle cells through inducible nitric oxide synthase iNOS-mediated processes, and macrophages that express CD68, a marker of M1 macrophages, are the first to invade injured muscle following acute injury |
|---|
| M1 macrophage | secretes | TNF |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells |
|---|
| M1 macrophage->M2 macrophage | transition | M2 macrophage |
Skeletal muscle |
17485518 |
| injured skeletal muscle recruits MOs exhibiting inflammatory profiles that operate phagocytosis and rapidly convert to antiinflammatory MPs that stimulate myogenesis and fiber growth |
|---|
| M2 macrophage | secretes | ARG1 |
Skeletal muscle |
28163303 |
| M2a macrophages secrete IL-10, and express CD206 and arginase 1 -ARG1-. |
|---|
| M2 macrophage | secretes | COL6A1 |
Skeletal muscle |
24232182 |
| For example, M2 macrophages secrete a more mature form of fibronectin and a higher amount of ColVI than do M1 macrophages [54,55]. The ECM proteins secreted by M2 macrophages are important components of the muscle stem cell niche and promote self-renewal of satellite cells [56,57]. |
|---|
| M2 macrophage | secretes | FN1 |
Skeletal muscle |
24232182 |
| For example, M2 macrophages secrete a more mature form of fibronectin and a higher amount of ColVI than do M1 macrophages [54,55]. The ECM proteins secreted by M2 macrophages are important components of the muscle stem cell niche and promote self-renewal of satellite cells [56,57]. |
|---|
| M2 macrophage | secretes | IGF1 |
Skeletal muscle |
20304951 |
| Macrophages also release mitogenic growth factors for myogenic cells and establish cell-cell interactions that protect myogenic cells from apoptosis. IL-4, IL-6, fibroblast growth factor, and IGF-1 as well as several other cytokines and growth factors influence myogenic cell behavior |
|---|
| M2 macrophage | secretes | IL10 |
Skeletal muscle |
28163303 |
| M2a macrophages secrete IL-10, and express CD206 and arginase 1 -ARG1-. |
|---|
| M2 macrophage | secretes | IL33 |
Skeletal muscle |
28163303 |
| This influence is further enhanced by the recruitment of Treg cells to regenerated muscle by IL-33 released by fibro-adipogenic progenitor -FAP- cells and possibly by macrophages. |
|---|
| M2 macrophage | secretes | IL4 |
Skeletal muscle |
20304951 |
| Macrophages also release mitogenic growth factors for myogenic cells and establish cell-cell interactions that protect myogenic cells from apoptosis. IL-4, IL-6, fibroblast growth factor, and IGF-1 as well as several other cytokines and growth factors influence myogenic cell behavior |
|---|
| M2 macrophage | secretes | TGFB1 |
Skeletal muscle |
28163303 |
| FAP cell proliferation and differentiation into cells with phagocytic or fibrogenic phenotypes are influenced by the release of transforming growth factor-beta -TGF beta- from macrophages and by IL-4 released by eosinophils. |
|---|
| Mast cell | secretes | Histamine |
Skeletal muscle |
17259966 |
| Mast cells... release histamine and other mediators after crosslinking of surface-bound IgE by allergen. |
|---|
| Mast cell | secretes | Histamine |
Skeletal muscle |
24232182 |
| Particularly, damage-activated mast cells almost instantly begin to secrete TNFa, histamine and tryptase and then initiate the de novo synthesis of other cytokines, such as interleukin (IL)6 |
|---|
| Mast cell | secretes | IL5 |
Skeletal muscle |
17259966 |
| The array of mediators released by human mast cells is enormous and explains how mast cells can be involved in so many different physiological and pathophysiological functions. Of particular relevance...cytokines, such as IL-3 -basophil recruitment and activation-, IL-5 -eosinophil recruitment and activation- and IL-13 -induction of IgE synthesis by B cells- |
|---|
| Mast cell | secretes | IL6 |
Skeletal muscle |
24232182 |
| Particularly, damage-activated mast cells almost instantly begin to secrete TNFa, histamine and tryptase and then initiate the de novo synthesis of other cytokines, such as interleukin (IL)6 |
|---|
| Mast cell | secretes | Leukotriene B4 |
Skeletal muscle |
17259966 |
| The array of mediators released by human mast cells is enormous and explains how mast cells can be involved in so many different physiological and pathophysiological functions. Of particular relevance in the pathogenesis of allergic inflammation are...LTB4, which targets neutrophils and mast-cell progenitors |
|---|
| Mast cell | secretes | TNF |
Skeletal muscle |
24232182 |
| Particularly, damage-activated mast cells almost instantly begin to secrete TNFa, histamine and tryptase and then initiate the de novo synthesis of other cytokines, such as interleukin (IL)6 |
|---|
| Mast cell | secretes | TPSAB1 |
Skeletal muscle |
24232182 |
| Particularly, damage-activated mast cells almost instantly begin to secrete TNFa, histamine and tryptase and then initiate the de novo synthesis of other cytokines, such as interleukin (IL)6 |
|---|
| Monocyte | secretes | IL1B |
Skeletal muscle |
24232182 |
| Indeed, Ly6C+ monocytes promote the recruitment of other monocytes by secreting proinflammatory cytokines, such as TNF-a and IL-1 |
|---|
| Monocyte | transition | M1 macrophage |
Skeletal muscle |
24232182 |
| Once monocytes have invaded the tissue, they begin to differentiate into macrophages. |
|---|
| Monocyte | secretes | TNF |
Skeletal muscle |
24232182 |
| Indeed, Ly6C+ monocytes promote the recruitment of other monocytes by secreting proinflammatory cytokines, such as TNF-a and IL-1 |
|---|
| MPO | stimulates | Damaged myofiber |
Skeletal muscle |
20219869 |
| LDL modification by MPO may be particularly important in regulating the process of tissue repair and regeneration in skeletal muscle; neutrophils that invade injured muscle in advance of M1 macrophages induce muscle membrane damage through the release of MPO. This may be one of several regulatory interactions that occur between neutrophils and macrophages during the early stage of muscle inflammation |
|---|
| MSTN | inhibits | Activated satellite->Myoblast |
Skeletal muscle |
12244043 |
| Myostatin is an inhibitor of myoblast differentiation and that this inhibition is mediated through Smad 3. |
|---|
| Myoblast | secretes | DLL1 |
Skeletal muscle |
17540178 |
| Immunostaining of isolated myofibers revealed that Delta-1 was expressed at high levels in Pax7+/Myf5+ satellite cells but low levels in Pax7+/Myf5- cells |
|---|
| Myoblast | transition | Myocyte->Myofiber |
Skeletal muscle |
22147605 |
| Upon myofiber culturing, the satellite cells proliferate, giving rise to satellite cell-derived myoblasts that can differentiate and form multinucleated myotubes |
|---|
| Myocyte->Myofiber | transition | Myofiber |
Skeletal muscle |
22147605 |
| Upon myofiber culturing, the satellite cells proliferate, giving rise to satellite cell-derived myoblasts that can differentiate and form multinucleated myotubes |
|---|
| Myofiber | inhibits | Activated FAP->Adipocyte |
Skeletal muscle |
20081842 |
| These results suggest that satellite cell-derived muscle fibres generate factors that strongly inhibit adipo- genic differentiation of PDGFRα+ cells. |
|---|
| Neutrophil | secretes | CCL2 |
Skeletal muscle |
24232182 |
| Neutrophils also secrete the chemokines MIP-1a, MCP-1 and others that favour the recruitment of monocytes |
|---|
| Neutrophil | secretes | CCL3 |
Skeletal muscle |
24232182 |
| Neutrophils also secrete the chemokines MIP-1a, MCP-1 and others that favour the recruitment of monocytes |
|---|
| Neutrophil | secretes | MPO |
Skeletal muscle |
20219869 |
| LDL modification by MPO may be particularly important in regulating the process of tissue repair and regeneration in skeletal muscle; neutrophils that invade injured muscle in advance of M1 macrophages induce muscle membrane damage through the release of MPO. This may be one of several regulatory interactions that occur between neutrophils and macrophages during the early stage of muscle inflammation |
|---|
| Neutrophil | secretes | TNF |
Skeletal muscle |
25374568 |
| Human and murine neutrophils also express and produce many TNF-superfamily members (Figure (Figure1A,B),1A,B), although at variable levels |
|---|
| nitric oxide | stimulates | Damaged myofiber |
Skeletal muscle |
20219869 |
| Furthermore, The expression of iNOS by M1 macrophages enables them to induce further muscle damage through production of cytotoxic levels of NO |
|---|
| nitric oxide | stimulates | Damaged myofiber |
Skeletal muscle |
18996917 |
| For example, macrophages that are driven in vitro to a pro-inflammatory, M1 phenotype lyse muscle cells through inducible nitric oxide synthase iNOS-mediated processes, and macrophages that express CD68, a marker of M1 macrophages, are the first to invade injured muscle following acute injury |
|---|
| Pericyte | secretes | ANGPT1 |
Skeletal muscle |
30016618 |
| However, experiments suggested that pericytes specifically express Ang-1 and IGF-1 to regulate MuSC activation and myofiber hypertrophy, respectively |
|---|
| Pericyte | secretes | IGF1 |
Skeletal muscle |
30016618 |
| However, experiments suggested that pericytes specifically express Ang-1 and IGF-1 to regulate MuSC activation and myofiber hypertrophy, respectively |
|---|
| Pericyte | transition | Myofiber |
Skeletal muscle |
21988915 |
| Here we show that pericytes, transgenically labelled with an inducible Alkaline Phosphatase CreERT2, but not endothelial cells, fuse with developing myofibres and enter the satellite cell compartment during unperturbed postnatal development |
|---|
| Pericyte | transition | Pericyte->Adipocyte |
Skeletal muscle |
25278877 |
| Skeletal muscle pericytes can differentiate in vitro toward adipogenic lineage (Farrington-Rock et al., 2004; Crisan et al., 2008a) but, like PDGFRα+ cells, do not generate myofibers, and only type-1 express PDGFRα. When purified type-1 pericytes are delivered intramuscularly in a mouse model of fatty infiltration, ectopic white fat is generated |
|---|
| Pericyte->Adipocyte | transition | Adipocyte |
Skeletal muscle |
25278877 |
| Skeletal muscle pericytes can differentiate in vitro toward adipogenic lineage (Farrington-Rock et al., 2004; Crisan et al., 2008a) but, like PDGFRα+ cells, do not generate myofibers, and only type-1 express PDGFRα. When purified type-1 pericytes are delivered intramuscularly in a mouse model of fatty infiltration, ectopic white fat is generated |
|---|
| Quiescent FAP | transition | Quiescent FAP->Activated FAP |
Skeletal muscle |
20081841 |
| These cells are quiescent in intact muscle but proliferate efficiently in response to damage. FAPs do not generate myofibres, but enhance the rate of differentiation of primary myogenic progenitors in co-cultivation experiments. In summary, FAPs expand upon damage to provide a transient source of pro-differentiation signals for proliferating myogenic progenitors |
|---|
| Quiescent FAP->Activated FAP | transition | Activated FAP |
Skeletal muscle |
20081841 |
| These cells are quiescent in intact muscle but proliferate efficiently in response to damage. FAPs do not generate myofibres, but enhance the rate of differentiation of primary myogenic progenitors in co-cultivation experiments. In summary, FAPs expand upon damage to provide a transient source of pro-differentiation signals for proliferating myogenic progenitors |
|---|
| Quiescent satellite | transition | Quiescent satellite->Activated satellite |
Skeletal muscle |
22493066 |
| In mature resting muscles, satellite cells are predominantly quiescent. Upon muscle injury, satellite cells are activated, enter the cell cycle, and proliferate |
|---|
| Quiescent satellite->Activated satellite | transition | Activated satellite |
Skeletal muscle |
22493066 |
| In mature resting muscles, satellite cells are predominantly quiescent. Upon muscle injury, satellite cells are activated, enter the cell cycle, and proliferate |
|---|
| TGFB1 | stimulates | Activated FAP->Fibroblast |
Skeletal muscle |
28163303 |
| FAP cell proliferation and differentiation into cells with phagocytic or fibrogenic phenotypes are influenced by the release of transforming growth factor-beta -TGF beta- from macrophages and by IL-4 released by eosinophils. |
|---|
| TGFB1 | stimulates | Activated FAP->Fibroblast |
Skeletal muscle |
26053624 |
| Taken together, this confirms that in addition to regulating their survival, TGFB1 also induces the differentiation of FAPs along the fibrogenic lineage |
|---|
| TNF | induces apoptosis | Activated FAP |
Skeletal muscle |
26053624 |
| In summary, our data show that inflammatory macrophages are both required for efficient FAP clearance by apoptosis in vivo and sufficient to induce their programmed cell death via a TNF-mediated mechanism in vitro. In addition, TNF-expressing macrophages are found in close proximity to FAPs during their clearance |
|---|
| TNF | induces apoptosis | Activated FAP |
Skeletal muscle |
28163303 |
| FAP cells are then eliminated by apoptosis that is driven by TNF released from M1-biased macrophages |
|---|
| TNF | stimulates | M0 macrophage->M1 macrophage |
Skeletal muscle |
25339958 |
| Albeit phagocytosis may provide the initial antigen stimulus, the activity of macrophages can be increased by cytokines secreted by helper T cells, with interferon gamma (IFN-) being one of the most potent macrophage activators |
|---|
| TNF | stimulates | Quiescent satellite->Activated satellite |
Skeletal muscle |
24232182 |
| At low physiological concentrations, TNF-a, tryptase and IL-6 promote activation and proliferation of satellite cells [31-33]. |
|---|
| TNF | stimulates | Quiescent satellite->Activated satellite |
Skeletal muscle |
24232182 |
| IL-1, IL-6 and TNF-a secreted by M1 macrophages are particularly important to induce proliferative effects on myogenic cells |
|---|
| TPSAB1 | stimulates | Myoblast |
Skeletal muscle |
21999702 |
| Our data show that tryptase can stimulate myoblast proliferation and this effect is part of a signaling cascade dependent on PAR-2 activation and on the downstream activation of COX-2 |
|---|
| TPSAB1 | stimulates | Quiescent satellite |
Skeletal muscle |
23813613 |
| Mast cells can also directly stimulate the proliferation of many cell types such as skeletal muscle, epithelial, and smooth muscle cells via tryptase, a serine protease only found in MCs and released after activation |
|---|
| TPSAB1 | stimulates | Quiescent satellite->Activated satellite |
Skeletal muscle |
24232182 |
| At low physiological concentrations, TNF-a, tryptase and IL-6 promote activation and proliferation of satellite cells [31-33]. |
|---|
| Treg | secretes | AREG |
Skeletal muscle |
28163303 |
| M1 macrophage populations then undergo a shift to a population that is biased towards the M2 pro-regenerative phenotype. Several ligands have important roles in promoting this phenotypic shift, including fibrinogen, amphiregulin -AREG- and interleukin-10 produced by regulatory T cells. |
|---|
| Treg | secretes | IL10 |
Skeletal muscle |
28163303 |
| M1 macrophage populations then undergo a shift to a population that is biased towards the M2 pro-regenerative phenotype. Several ligands have important roles in promoting this phenotypic shift, including fibrinogen, amphiregulin -AREG- and interleukin-10 produced by regulatory T cells. |
|---|
| WISP | stimulates | Activated satellite->Myoblast |
Skeletal muscle |
30686765 |
| WISP1 is required for efficient muscle regeneration and controls the expansion and asymmetric commitment of MuSCs through Akt signaling |
|---|